Blog
Fish Consumption, Brain Mercury, and Neuropathology in Patients With Alzheimer Disease and Dementia
follow us on twitter: @GoAfricaNetwork ,@DocSamuelJones
JAMA
The number of older adults with Alzheimer disease or other dementia will increase worldwide over the coming decades. Notably, in China and other Asian countries where a large population is living longer, Alzheimer disease and dementia have become a major public health concern.1 There is a pressing need to identify preventive strategies for Alzheimer disease and dementia,1 such as the potential role of dietary intake. For instance, the Mediterranean-style diet (rich in fruit, vegetables, legumes, cereals, and olive oil and including some poultry, little red meat, and regular fish intake) has been associated with better cognitive health and a decreased risk of Alzheimer disease or dementia in observational studies.2,3Consumption of fatty fish and fish oils has been associated with cognitive benefits—particularly for neurocognitive development among infants and children.4 Intakes of fish or n-3 fatty acids have also been consistently associated with the slowing of cognitive decline and decreased risk of Alzheimer disease and dementia in older adults.5,6
However, results from large randomized clinical trials (RCTs) are needed before recommending a Mediterranean-style diet, increased fish consumption, or supplementation with n-3 fatty acids to improve cognitive health.7 Initial RCTs of dietary interventions against cognitive decline or risk of Alzheimer disease or dementia have shown conflicting results.7 A possible reason for this inconsistency may be related to the fact that diet is frequently correlated with other lifestyle characteristics influencing cognitive health.7 On this assumption and among 1260 at-risk older individuals, the FINGER study compared a multidomain intervention that combined physical exercise, cognitive stimulation, monitoring of vascular risk factors (notably hypertension), and diet vs control participants who received general health advice and showed improvement or preservation of cognitive functioning in the intervention group at 2 years.8
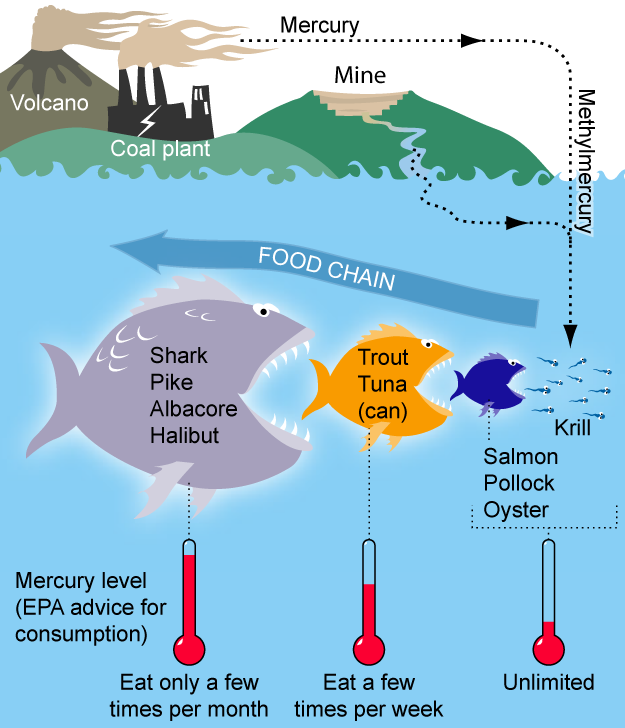
Until clear recommendations for dietary interventions (from RCTs) are available, many people may consider fish and n-3 fatty acids as a potential strategy to prevent cognitive decline and other health problems, resulting in more fish and fish oil intake. One concern with consumption of fish and fatty acids, however, has been mercury contamination. Given the neurotoxicity of mercury, its association with Alzheimer disease or dementia has remained as a concern,9 although observational studies have failed to show that increased levels of mercury in the brain, serum, or blood are associated with increased risk of Alzheimer disease or dementia.
In this issue of JAMA, Morris and colleagues10 present important results from the neuropathological evaluation of participants of the Rush Memory and Aging Project (MAP) study, which may help alleviate some of these concerns. In this cross-sectional study, the autopsied brains of 286 deceased MAP participants (mean age at death, 89.9 years; 67% women) were assessed regarding dementia-related pathology including Alzheimer disease, Lewy bodies, and the number of macroinfarcts and microinfarcts. Mercury and selenium concentration in brain tissue also was measured. In addition, participants in this study completed food frequency questionnaires (mean interval, 4.5 years before death) on consumption of seafood and n-3 fatty acids. Seafood consumption in this sample was moderate, with means of 1.3 seafood meals per week in the lowest tertile and 2.7 seafood meals per week in the highest.
The authors found that moderate seafood consumption of at least 1 meal per week was positively correlated with brain mercury levels, but higher brain levels of mercury were not correlated with more Alzheimer disease or dementia brain pathology. This latter finding is reassuring because ingested mercury accumulates in the body over decades and brain levels hence result from exposure, which likely precedes any Alzheimer disease or dementia development. This appears to be the first study showing an absence of an increased risk of Alzheimer disease or dementia related to mercury based on the level of brain pathology, suggesting that seafood can be consumed without substantial concern of mercury contamination diminishing its possible cognitive benefit in older adults.
Morris et al10 also established the relationship of the frequency of seafood consumption, assessed by dietary questionnaires, and derived levels of fatty acids with brain neuropathology in deceased participants of the MAP Project. Higher intake levels of α-linoleic acids were correlated with lower risk of cerebral infarcts, confirming current understanding of the cardiovascular benefits of α-linoleic acid. There was no correlation between reported use of fish oil supplements and brain neuropathology, which might be explained by their short-term or inconsistent use but may also be consistent with negative results of clinical trials on fish oil supplementation.11 The study also contributes important knowledge by showing beneficial correlations between intake of seafood or derived levels of n-3 fatty acids and brain neuropathology in which seafood consumption (≥1 meal/week) was correlated with less Alzheimer disease neuropathology. However, this finding was limited to participants who were positive for the apolipoprotein E (APOE) ε4 allele, with a statistically significant modification term. These results suggest the possibility of lack of statistical power as an explanation for the absence of a correlation in non-APOE ε4 carriers. However, the estimates for the β-coefficients of the regressions of seafood or the derived docosahexaenoic acid plus eicosapentaenoic acid (DHA + EPA) food sources on the 4 measures of Alzheimer disease brain pathology (article, Table 4) differ considerably between APOE ε4 carriers and noncarriers, and the majority (76.4%) of the study sample (and population) are APOE ε4 negative. These differences in the correlations between fish or n-3 fatty acids and Alzheimer disease or dementia brain pathology, according to APOE ε4 status, underscore the present limits in understanding Alzheimer disease and other dementias resulting from neurodegenerative processes.
Research and debates are ongoing about the role of the APOE ε4 allele and other genes (eg, the cholesterol-regulating gene for 3-hydroxy-3-methylglutaryl-CoA reductase [HMGCR])—a powerful genetic modifier for risk, age of onset, and conversion from mild cognitive impairment to Alzheimer disease.12 At the same time, amyloid deposition in the brain may be more complicated to relate to clinical disease and its symptoms than previously thought.13,14 Other protein deposits appear to be important such as the TAR DNA-binding protein 43, which has recently been related to Alzheimer disease.15 A combination of imaging studies, pathological studies (eg, MAP), a better understanding of the genetic underpinnings of neurodegenerative pathologies, and robust epidemiological studies are needed to clarify and refine current concepts. Such research may also facilitate the currently stalled process of developing pharmacological interventions for Alzheimer disease and other dementias.
Amyloid deposits and neurofibrillary tangles continue to be the pathological hallmarks at least for Alzheimer disease dementia. This is why Morris et al10 chose to analyze correlations with Alzheimer disease or other dementia brain pathology as opposed to clinical Alzheimer disease or dementia diagnoses. Preliminary results from the MAP study on the association between fish or fatty acids and cognitive decline have been presented.16 Ultimately, proof of the brain pathological concepts of Alzheimer disease and other dementias will be based on data from clinical trials confirming that preventive or therapeutic interventions on these elements of brain neuropathology will reduce clinical manifestations of Alzheimer disease and other dementias.
In the meantime, patients and their families may be hopeful that interventions such as seafood consumption may help reduce clinical manifestations of Alzheimer disease or dementia, and the report by Morris et al10provides reassurance that seafood contamination with mercury is not related to increased brain pathology. Although food questionnaires were only available for the last 4.5 years before death in this study sample, mercury was strongly correlated with fish consumption, which is indeed the main source of body mercury in North America. This result may thus confirm that the seafood consumption measured in the sample is representative of long-term eating habits, likely preceding the development of cognitive decline. This seafood consumption was, in turn, significantly correlated with less Alzheimer disease pathology according to 4 measures among participants carrying the APOE ε4 allele. Eating fatty fish may continue to be considered potentially beneficial against cognitive decline in at least a proportion of older adults, a strategy that now generally should not be affected by concerns about mercury contamination in fish. Such a simple strategy is encouraging in the light of the lack of evidence on protection against many neurodegenerative diseases such as Alzheimer disease and Parkinson disease, another cause of dementia.17